The most recent report from the CDC (released in 2021) reveals that nearly 12% of the U.S. population has diabetes. Diabetic retinopathy (DR), a common complication of diabetes mellitus (DM), affects approximately 30% of adults with diabetes and is the leading cause of blindness in working-aged Americans.
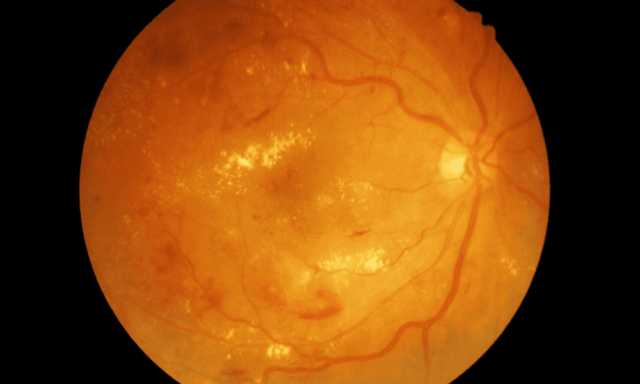
The International Clinical Diabetic Retinopathy (ICDR) Severity Scale was created to refine DR classification in efforts to improve diagnosis and management:
- Mild NPDR: Microaneurysms only → Annual monitoring.
- Moderate NPDR: Intraretinal hemorrhages present → 9- to 12-month follow-up.
- Severe NPDR: Based on the 4-2-1 rule (four quadrants of hemorrhaging, two quadrants of venous beading, one quadrant of IRMA) → Referral to retina specialist recommended.
- PDR: Presence of neovascularization → Urgent referral for anti-VEGF therapy and/or panretinal photocoagulation (PRP).
- DME: Referral recommended for center-involved (CI-DME) cases, particularly those affecting best-corrected visual acuity (BCVA).
During “Current Strategies on Managing Diabetic Eye Disease,” a session at the recent Vision Expo East, Mary Beth Yackey, OD, and Jessica Haynes, OD, presented strategies for managing DR in your practice — tackling patient education, risk assessment, and treatment coordination for your diabetic patients. We’ll touch on a few of the guidelines shared:
- Type 1 Diabetes: The American Diabetes Association and AOA guidelines recommend a baseline eye exam within five years of diagnosis and annual follow-ups thereafter.
- Type 2 Diabetes: Since undiagnosed diabetes is common, patients should have a comprehensive eye exam at diagnosis, with follow-up intervals based on DR severity.
- For moderate-to-severe NPDR, consider additional OCT, OCT-A, or electroretinography (ERG) to assess progression risk. In cases of rapid disease progression, poor glycemic control, or noncompliance, earlier referral may be warranted.
Recommended resource: Diabetic Eye Disease: A Comprehensive Look at the Optometrist’s Role
The doctors also spoke to new therapeutic treatments that are enhancing DR and diabetic macular edema (DME) management:
- Anti-VEGF injections act as first-line therapy for CI-DME and proliferative diabetic retinopathy (PDR); newer agents like faricimab and high-dose aflibercept offer longer durability.
- Panretinal photocoagulation (PRP) remains the gold standard for high-risk PDR to reduce neovascularization.
- Intravitreal corticosteroid implants may benefit pseudophakic patients or those unresponsive to anti-VEGF treatment.
- Emerging therapies: Fenofibrate (lipid-lowering agent) has shown promise in slowing DR progression, while nutritional supplementation targeting oxidative stress is an evolving area of research.
Patient education points to make
Consider the following information, as outlined in the VEE presentation, when discussing things with your patients:
After 15 years of disease duration, 80% of patients with type 1 DM will have some degree of retinopathy.
Elevated blood glucose levels and HbA1c values (less than or equal to 7%), as well as less glucose time in range assessed by continuous glucose monitoring devices, are also associated with higher rates of retinopathy.
Control of blood pressure, lipids, and management of comorbidities, such as sleep apnea, all reduce risk of progression.
Pregnancy in diabetics places increase risk of progression to severe retinopathy; however this is not the case in those with gestational diabetes.
Glucagon-like peptide-1 (GLP-1) receptor analogs are a newer, highly effective category of medication for diabetes management including semaglutide (Ozempic and Wegovy, both Novo Nordisk), and tirzepatide (Mounjaro, Eli Lilly).
Although improved glycemic control is encouraged for promotion of long-term positive outcomes, a transient worsening of retinopathy may be seen initially. (Likely related to VEGF expression, reactive oxygen species production and breakdown of the blood-retinal barrier.)
Source: “Current Strategies on Managing Diabetic Eye Disease,” presented by Mary Beth Yackey, OD, Jessica Haynes, OD, at Vision Expo East; Feb 19-22, 2025; Orlando.
This content is intended for educational purposes only and does not substitute for clinical judgment. Treatment decisions should be based on individual patient needs, professional guidelines, and a comprehensive clinical evaluation.

![A Practical Guide to Presbyopia Drops [UPDATED]](https://optometry.industry411.com/wp-content/uploads/2025/05/guide-to-presbyopia-drops-238x178.png)


